
Vaccsbook

Infectious Diseases . . . and How to Avoid Them
Ticks and Lyme Disease

This information is for entertainment purposes only. It has not been verified by a third party. Last updated: 2024-Mar-15.
Ticks are insects that bite other living species, commonly humans, dogs, sheep, and cattle, to suck their blood.
Ticks do not cause infection directly, but carry bacteria or viruses which they inject when biting a host.
They have a tiny head in between two antenna, a large body covered by a decorative "dorsal shield", and three pairs of legs.
Adult male ticks may attach and bite, but rarely suck blood and transmit disease.
If a tick is identified as a female, then there is a risk of disease transmission.
Regardless of species, the decorative shield on the back of females will cover only a small portion (left side of above), while that of males will cover almost the entire body.
Tick-related diseases (usually) involve:
However, ticks rarely jump from reservoir to host, but are acquired by the host from tall grass, straw, scrub, or fallen leaves. Ticks detect potential human hosts by sensing odours rather than by eyesight.
A tick must usually attach to the skin for several hours before transmitting disease. Frequent surveillance from head to toe after possible exposure, and correct removal (see below) can prevent disease.

or fine-tipped tweezers placed on the skin either side of the tick's head.
Once removed, trap the tick under a drinking glass, and confirm it has the appearance of a female Deer tick. If possible take a close-up high resolution photo and forward this to public health or local tick surveillance facility for further confirmation.
Lyme Disease
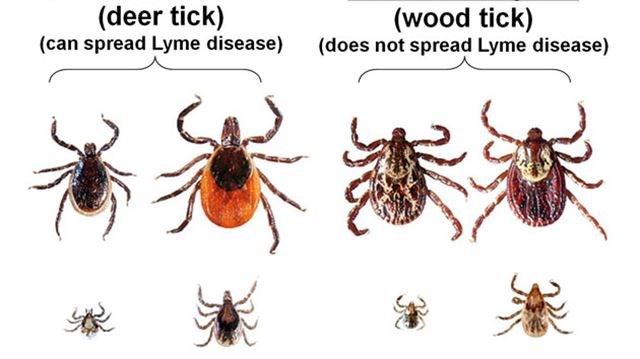
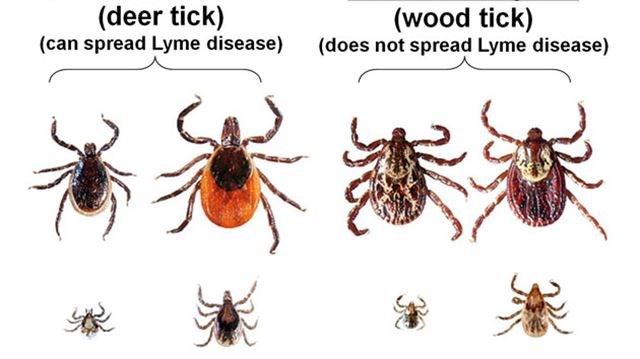
Is it a Deer Tick . . or a Wood Tick ?
Signs and Symptoms
The initial tick bite is usually asymptomatic.
10 days after the bite a rash appears at the site of the bite and gradually enlarges over the following 4 weeks.

Untreated, the bacteria then spreads to the joints, heart, nervous system and other areas of the skin.
Joint symptoms comprise pain and swelling.
Heart involvement can result in an unusually slow heart rate and inflammation of the heart muscle, causing chest pain and shortness of breath.
Neurological involvement can result in meningitis causing headache, fever and confusion, and also result in skin sensations of pain, numbness or tingling, or paralysis of individual muscles.
The rash can spread to other areas of the skin, but is usually smaller than the original.
In a minority of patients, some of the above symptoms can last for several years.
Treatment
If the tick is still on the skin, initial treatment requires careful removal of the tick, , and confirmation that it is a Deer Tick.
It is generally believed that the tick must be on human skin for 24 hours before they bite. However, these ticks tend to hide (and cling) in hair and skin creases, and are not automatically washed off in the shower.
If in doubt, see a physician immediately for a single dose of antibiotics, usually Amoxicillin or Doxycycline - "docks-ee-sike-lin".
Once the rash or other characteristic symptoms occur, a prolonged course of (the same) antibiotics is indicated, initially given intraveneously if symptoms are severe.
Rocky Mountain Spotted Fever (RMSF) also called Colorado Tick Fever
Symptoms
Symptoms occur within a week of the tick bite and comprise fever, chills, severe headache, red eyes, muscle aches, and after a few days, a non-itchy characteristic rash that starts on the extremities and later spreads to the body.

Untreated it can progress to severe inflammation of the brain, heart, lungs, and kidneys, and is often fatal.
Treatment
The tick can be on the host for only 6 hours before injecting the bacteria. If seen, it should be removed as described above.
If RMSF is suspected on the basis of symptoms, and/or in a location known to have the tick, antibiotics such as Doxycycline should be started immediately.
Tularemia
Symptoms
Symptoms occur within a week of the tick bite and comprise fever, chills, severe headache, muscle aches, fatigue, abdominal pain, nausea and vomiting.
In some cases, a dry cough and pain with breathing may occur.
Signs may include an ulcer at the site of the bite, and swollen lymph nodes close by.
Treatment
Diagnosis can be a challenge; it is usually based on the above symptoms and probable exposure to a reservoir.
Treatment is with antibiotics such as Doxycycline or Ciprofloxacin.
STARI, southern tick-associated rash illness
Symptoms
Symptoms consist of a circular, expanding rash, usually accompanied by fatigue, headache, fever, and muscle pains.
Treatment
Symptoms invariably resolve with oral Doxycyline. Unlike Lyme disease, chronic symptoms do not develop.
Human Monocytic Ehrlichiosis.
Symptoms
Symptoms occur within a 1-2 weeks of the tick bite, starting with fevere, headache, fatigue, low back pain. Some patients will also develop joint pain, muscle aches, cough, sore thoat, abdominal pain, nausea and vomiting, and confusion.
Erlichosis can be fatal in about 1% of patients.
Treatment
Diagnosis should be suspected on the above symptoms, and confirmed by laboratory tests for bacterial DNA and antibodies.
Treatment is with Doxycycline which should be started if Erlichoisis is suspected, without waiting for laboratory confirmation.
Babesiosis
Symptoms
Babeosis invades red blood cells and causes symptoms of fever, fatigue, weakness, and shortness of breath. In rare severe cases, usually those with poor immune systems and/or prior spleen removal, death can occur due to failure of multiple organs.
Treatment
Once diagnosis is confirmed by examining blood cells under a microscope, antibiotics such as Clindamycin are usually effective.
Anaplasmosis
Symptoms
In humans, symptoms develop 1-6 weeks after initial infection.
Early symptoms are fever & chills, headache, muscle aches, nausea and vomiting.
Without treatment, severe symptoms including respiratory and kidney failure may occur and occasionally result in death. This is more common in young children, the elderly, and the immunocompromised.
Diagnosis
Diagnosis is suspected by symptoms and a history of tick exposure and/or bite.
Diagnosis can be confirmed by a bloodtest for antibodies to the Anaplasma phagocytophilum bacterium; however this may take several weeks to process conclusively.
Microscopic examination of blood smear may indicate the diagnosis, but is not sensitive or specific.
Treatment
Doxycycline should be started immediately if Anaplasmosis is suspected. The CDC states this is safe to use in children under 8 years, fears of permanent teeth discolouration which occurred with older tetracyclines have not beeen shown to occur with Doxycycline.
(Doxyxycline is often effective against other tick-borne infections.)
Powassan Virus
Symptoms
Most people develop mild or no symptoms. If symptoms do occur, it is usually from one week to one month after the tick bite, and comprise fever, seizures, weakness, confusion, headache, and memory loss. Rarely these progress to full-blown encephalitis and meningitis, then with a fatality rate of about 10%.
Diagnosis
Diagnosis is made on the history of a tick bite, plus laboraty tests of blood or spinal fluid for antibodies.
Treatment
Treatment in severe cases requires hospitalization for IV hydration and occasionally ventilation; there is no specific anti-viral medication.
Carefully controlled lab experiments using freezers, show that ticks will die between -18°C and -10°C. But in their natural habitat, ticks can adapt to cold temperatures in various ways; e.g. on a host animal or by going dormant under leaves and debris.
Lyme disease was first identified 50 years ago. Since then global temperatures have supposedly increased 0.4°C to 0.6°C (although global temperatures actually dropped between 2000 and 2015). This increase is minimal when compared to the temperature range at which ticks may die.
Any current or future increase in diagnoses of tick-borne human disease is most probably due to increased awareness on the part of patients and clinicians, rather than any change in climate.
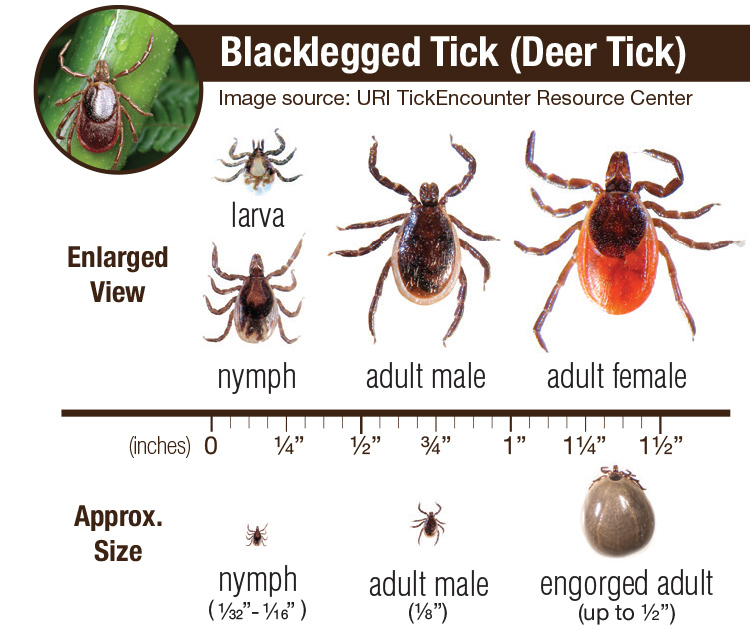
General Appearance
Ticks are large enough to be seen by the naked eye, usually about 2mm, but can be five times that if they have just bitten, and have become engorged with, the blood of their victim.They have a tiny head in between two antenna, a large body covered by a decorative "dorsal shield", and three pairs of legs.
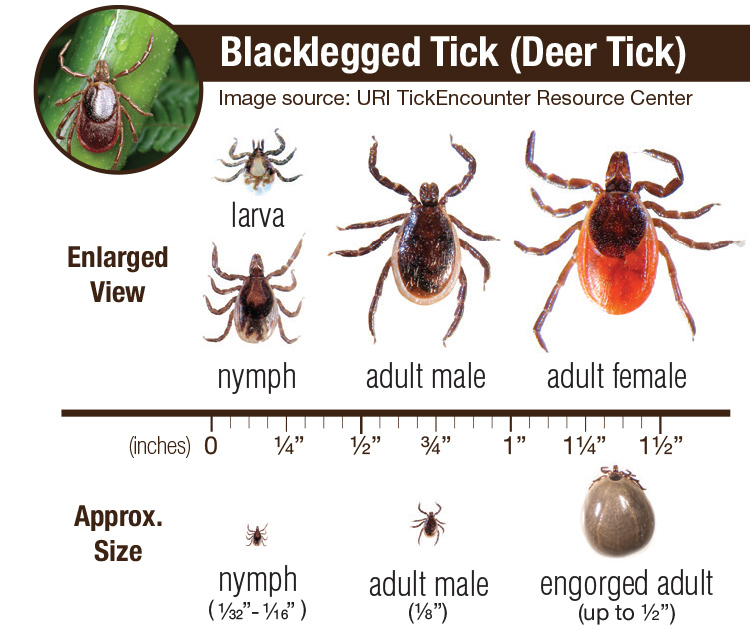
Ticks are "Binary"
Determination of a tick's sex is important.Adult male ticks may attach and bite, but rarely suck blood and transmit disease.
If a tick is identified as a female, then there is a risk of disease transmission.
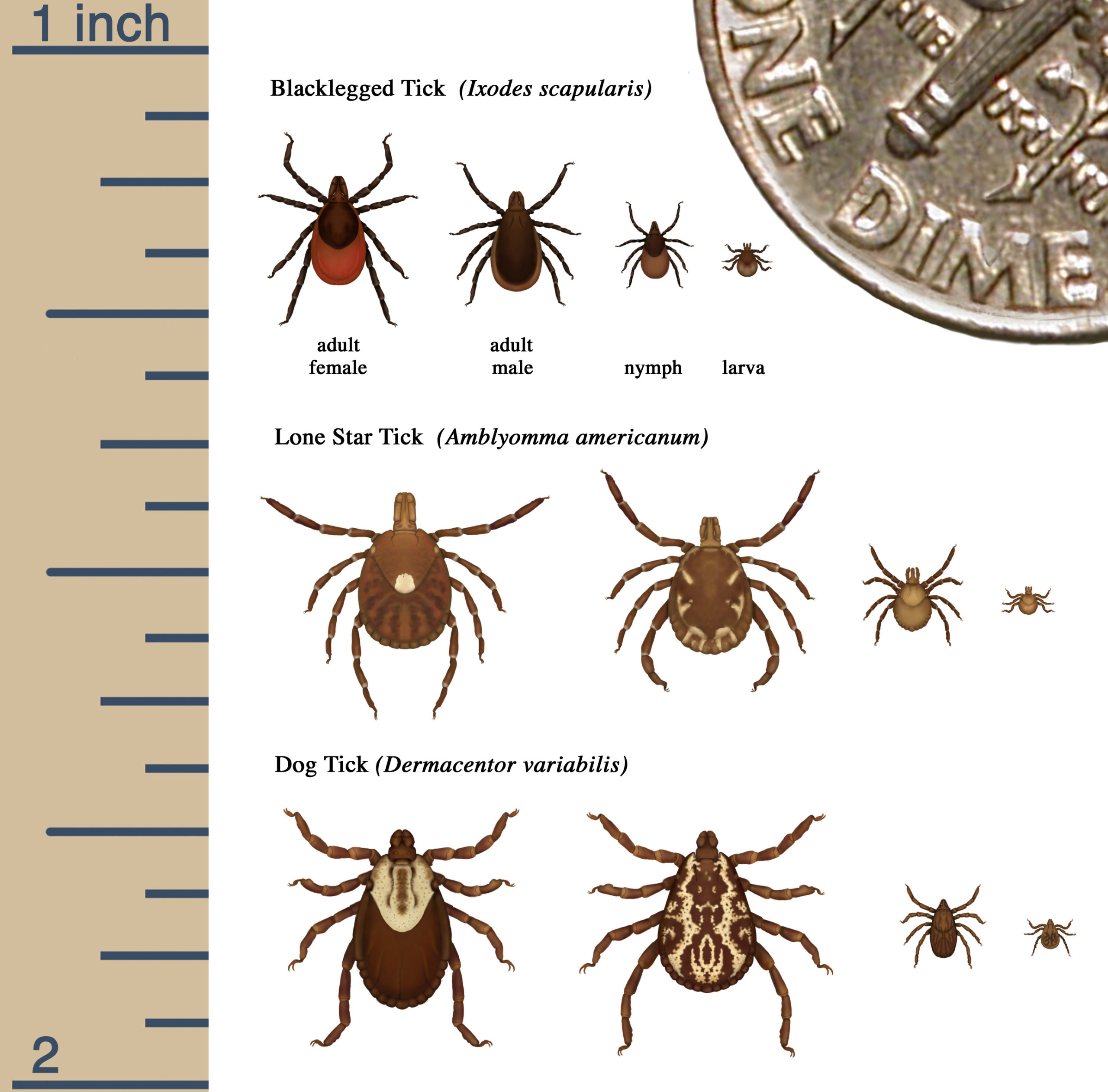
Regardless of species, the decorative shield on the back of females will cover only a small portion (left side of above), while that of males will cover almost the entire body.
Tick-related diseases (usually) involve:
- A Reservoir, an animal on which the tick can live without causing disease to that animal.
- A Vector, the tick itelf.
- An Agent, the bacteria or virus which the tick injects.
- A Host, the human or animal infected.
However, ticks rarely jump from reservoir to host, but are acquired by the host from tall grass, straw, scrub, or fallen leaves. Ticks detect potential human hosts by sensing odours rather than by eyesight.
A tick must usually attach to the skin for several hours before transmitting disease. Frequent surveillance from head to toe after possible exposure, and correct removal (see below) can prevent disease.
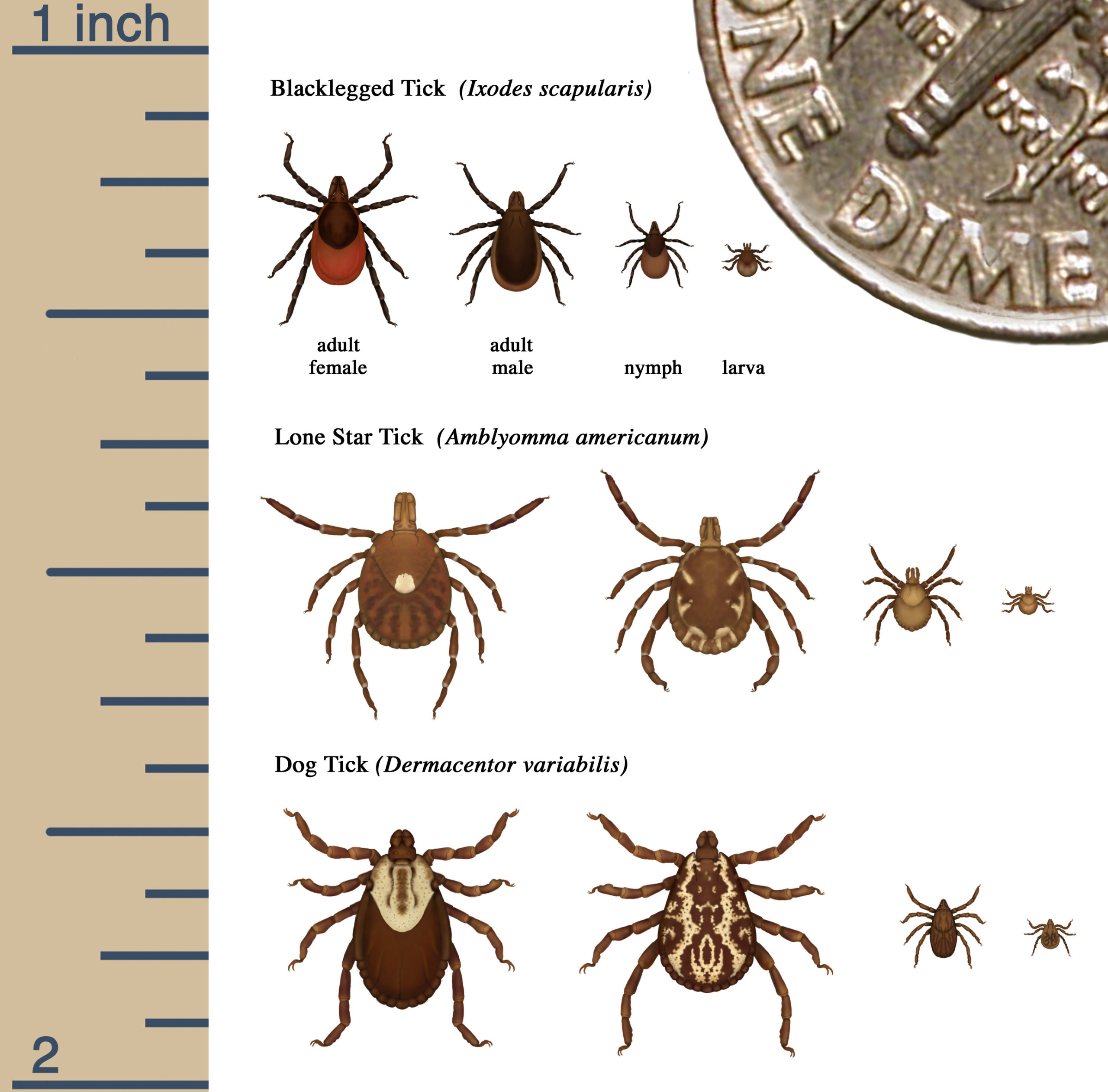
Common Types of Tick
| Common Name | Scientific Name | Geography | Human Diseases |
|---|---|---|---|
| American Dog or Wood Tick | Dermacentor variabilis | Northeast US and southeast Canada | Rocky Mountain Spotted Fever, Tularemia |
| Eastern Blacklegged aka Deer Tick | Ixodes scapularis | NE USA and SE Canada | Lyme, Babeosis, Ehrlichiosis, Powassan Virus |
| Lone Star Tick | Amblyomma americanum | Southeast USA, spreading to Eastern USA and Canada | STARI, "southern tick-associated rash illness", Ehrlichiosis, Anaplasmosis, (not Lyme) |
| Brown Dog Tick | Rhipicephalus sanguineus | West coast USA | Rocky Mountain Spotted Fever |
| Western Blacklegged Deer Tick | Ixodes pacificus | West coast USA & Canada | Lyme, Babeosis |
| Rocky Mountain Wood Tick | Dermacentor andersoni | Rocky Mountain states, USA | Rocky Mountain Spotted Fever |
| Squirrel Tick | Ixodes marxi | Throughout USA and Canada | Powassan Virus (not Lyme) |
| Groundhog/Woodchuck Tick | Ixodes cokei | Eastern half of USA and Canada | Powassan Virus |
Ticks Removal
If a tick is found, it is vital to remove the tick's head (the part which does the biting) from the skin. This can be done with (cheap) purpose-designed tools
or fine-tipped tweezers placed on the skin either side of the tick's head.
Once removed, trap the tick under a drinking glass, and confirm it has the appearance of a female Deer tick. If possible take a close-up high resolution photo and forward this to public health or local tick surveillance facility for further confirmation.
Diseases in Humans
Multiple human diseases have been identified, a sample of those in the industrialized world are given below.Lyme Disease
- Reservoir: White-tailed deer and many small rodents.
- Vector: Deer tick (Ixodes species "icks-oh-deez")
- Agent: Borella Burgdorferi "Bore-rella Burg-door-fer-ree" (bacteria), and other Borella species..
- Hosts: Humans, dogs, cats.
Is it a Deer Tick . . or a Wood Tick ?
Signs and Symptoms
The initial tick bite is usually asymptomatic.
10 days after the bite a rash appears at the site of the bite and gradually enlarges over the following 4 weeks.

Untreated, the bacteria then spreads to the joints, heart, nervous system and other areas of the skin.
Joint symptoms comprise pain and swelling.
Heart involvement can result in an unusually slow heart rate and inflammation of the heart muscle, causing chest pain and shortness of breath.
Neurological involvement can result in meningitis causing headache, fever and confusion, and also result in skin sensations of pain, numbness or tingling, or paralysis of individual muscles.
The rash can spread to other areas of the skin, but is usually smaller than the original.
In a minority of patients, some of the above symptoms can last for several years.
Treatment
If the tick is still on the skin, initial treatment requires careful removal of the tick, , and confirmation that it is a Deer Tick.
It is generally believed that the tick must be on human skin for 24 hours before they bite. However, these ticks tend to hide (and cling) in hair and skin creases, and are not automatically washed off in the shower.
If in doubt, see a physician immediately for a single dose of antibiotics, usually Amoxicillin or Doxycycline - "docks-ee-sike-lin".
Once the rash or other characteristic symptoms occur, a prolonged course of (the same) antibiotics is indicated, initially given intraveneously if symptoms are severe.
Rocky Mountain Spotted Fever (RMSF) also called Colorado Tick Fever
- Reservoir: Rodents.
- Vector: A Wood tick (Dermacentor andersoni) or Dog tick (Dermacentor variabilis)
- Agent: Rickettsia rickettsii (bacteria)
- Hosts: Humans, dogs (usually mild symptoms).
- Locations: US rocky mountains, above 4,000 feet.
Symptoms
Symptoms occur within a week of the tick bite and comprise fever, chills, severe headache, red eyes, muscle aches, and after a few days, a non-itchy characteristic rash that starts on the extremities and later spreads to the body.

Treatment
The tick can be on the host for only 6 hours before injecting the bacteria. If seen, it should be removed as described above.
If RMSF is suspected on the basis of symptoms, and/or in a location known to have the tick, antibiotics such as Doxycycline should be started immediately.
Tularemia
- Reservoir: Mice,squirrels, rabbits..
- Vector: A Wood tick (Dermacentor andersoni) or Dog tick (Dermacentor variabilis).
- Agent: Francisella tularensis (bacteria)
- Hosts: Humans, sheep, dogs, cats.
Symptoms
Symptoms occur within a week of the tick bite and comprise fever, chills, severe headache, muscle aches, fatigue, abdominal pain, nausea and vomiting.
In some cases, a dry cough and pain with breathing may occur.
Signs may include an ulcer at the site of the bite, and swollen lymph nodes close by.
Treatment
Diagnosis can be a challenge; it is usually based on the above symptoms and probable exposure to a reservoir.
Treatment is with antibiotics such as Doxycycline or Ciprofloxacin.
STARI, southern tick-associated rash illness
- Reservoir: White-tailed deer.
- Vector: Lone Star Tick.
- Agent: Borrleia lonestar (possibly, research underway).
- Hosts: Humans, domestic dogs and cats,
- Location: Gulf of Mexico, Lower Great Lakes, Eastern USA upto Maine
Symptoms
Symptoms consist of a circular, expanding rash, usually accompanied by fatigue, headache, fever, and muscle pains.
Treatment
Symptoms invariably resolve with oral Doxycyline. Unlike Lyme disease, chronic symptoms do not develop.
Human Monocytic Ehrlichiosis.
- Reservoir: White-tailed deer (possibly domestic dogs and goats, racoons, and coyotes).
- Vector: Lone Star Tick and Blacklegged tick
- Agent: Ehrlichia chaffeensis, Ehrlichia ewingii, Ehrlichia muris eauclairensis (bacteria)
- Hosts: Humans
- Location: Gulf of Mexico to Great Lakes, Eastern USA upto Maine
Symptoms
Symptoms occur within a 1-2 weeks of the tick bite, starting with fevere, headache, fatigue, low back pain. Some patients will also develop joint pain, muscle aches, cough, sore thoat, abdominal pain, nausea and vomiting, and confusion.
Erlichosis can be fatal in about 1% of patients.
Treatment
Diagnosis should be suspected on the above symptoms, and confirmed by laboratory tests for bacterial DNA and antibodies.
Treatment is with Doxycycline which should be started if Erlichoisis is suspected, without waiting for laboratory confirmation.
Babesiosis
- Reservoir: White-footed mouse.
- Vector: Ixodes scapularis (one of the ticks which also causes Lyme disease).
- Agent: Babesi Microti, Babesia divergens, (many other species of Babesia bacteria).
- Hosts: Humans, cattle, dogs, and less seriously almost all other mammals.
Symptoms
Babeosis invades red blood cells and causes symptoms of fever, fatigue, weakness, and shortness of breath. In rare severe cases, usually those with poor immune systems and/or prior spleen removal, death can occur due to failure of multiple organs.
Treatment
Once diagnosis is confirmed by examining blood cells under a microscope, antibiotics such as Clindamycin are usually effective.
Anaplasmosis
- Reservoir: White-footed mouse, deer,.
- Vector: Blacklegged ticks (Ixodes scapularis and Ixodes pacificus).
- Agent: Anaplasma phagocytophilum (bacterium)
- Hosts: Humans, cats, dogs, sheep, goats, cows, horses.
- Locations: Worldwide, throught USA and Canada but less so in the Great Plains
Symptoms
In humans, symptoms develop 1-6 weeks after initial infection.
Early symptoms are fever & chills, headache, muscle aches, nausea and vomiting.
Without treatment, severe symptoms including respiratory and kidney failure may occur and occasionally result in death. This is more common in young children, the elderly, and the immunocompromised.
Diagnosis
Diagnosis is suspected by symptoms and a history of tick exposure and/or bite.
Diagnosis can be confirmed by a bloodtest for antibodies to the Anaplasma phagocytophilum bacterium; however this may take several weeks to process conclusively.
Microscopic examination of blood smear may indicate the diagnosis, but is not sensitive or specific.
Treatment
Doxycycline should be started immediately if Anaplasmosis is suspected. The CDC states this is safe to use in children under 8 years, fears of permanent teeth discolouration which occurred with older tetracyclines have not beeen shown to occur with Doxycycline.
(Doxyxycline is often effective against other tick-borne infections.)
Powassan Virus
- Reservoir: Multiple, including skunks, weasels, woodchucks, groundhogs, squirrels, raccoons, foxes, and mice.
- Vector: Squirrel tick, Groundhog tick, and Blacklegged tick
- Agent: Powassan Virus
- Hosts: Humans
- Locations: Northeastern US, Great Lakes, rarely in Canada (despite the first ever case being discovered in Powassan, Ontario).
Symptoms
Most people develop mild or no symptoms. If symptoms do occur, it is usually from one week to one month after the tick bite, and comprise fever, seizures, weakness, confusion, headache, and memory loss. Rarely these progress to full-blown encephalitis and meningitis, then with a fatality rate of about 10%.
Diagnosis
Diagnosis is made on the history of a tick bite, plus laboraty tests of blood or spinal fluid for antibodies.
Treatment
Treatment in severe cases requires hospitalization for IV hydration and occasionally ventilation; there is no specific anti-viral medication.
Ticks . . . and Climate Change
Ticks can survive cold winters; some studies show only around 20 percent of the population die off.Carefully controlled lab experiments using freezers, show that ticks will die between -18°C and -10°C. But in their natural habitat, ticks can adapt to cold temperatures in various ways; e.g. on a host animal or by going dormant under leaves and debris.
Lyme disease was first identified 50 years ago. Since then global temperatures have supposedly increased 0.4°C to 0.6°C (although global temperatures actually dropped between 2000 and 2015). This increase is minimal when compared to the temperature range at which ticks may die.
Any current or future increase in diagnoses of tick-borne human disease is most probably due to increased awareness on the part of patients and clinicians, rather than any change in climate.